Birinci basamakta nörolojik hastalarda Teletıp kullanımı
COVID-19 pandemisi, sağlık hizmeti sunumunda birçok olumsuz etkinin yanı sıra, yeni gelişmelere de neden oldu. Bu gelişmelerden biri teletıp ve dijital sağlık çözümlerinin uygulanmasıdır. Sağlık hizmetlerine erişimdeki eşitsizlikler ve nöroloji alanında yeterli uzman gücün eksikliği nedeniyle, dünya çapında büyük kitleler nörolojik tıbbi bakıma erişmede zorluklar yaşamaktadır. Mevcut araştırmalara göre, sıkça görülen nörolojik şikayetlerle karşılaşan hastalar genellikle aile hekimlerine başvurma eğilimindedir. Bu derlemenin amacı, teletıp ortamında nörolojik değerlendirme prensiplerini vurgulamak, nörologlar ve aile hekimlerinin sağlık hizmeti sunumundaki rollerini ortaya koymak ve sorun çözme yaklaşımıyla tele-nörolojideki gelişmelere değinmektir.
Tam Metin
Introduction
The rapid development of information and communication technologies in the 21st century has also affected the concept of doctor-patient consultations, and theoretical studies under the title of telemedicine have begun to materialize in medical literature.(1,2) In order to prevent the spread of the disease in the COVID-19 pandemic, prohibitions were implemented, and non-emergency outpatient services were suspended.(3) In this period, some private and public service providers on a global scale took the initiative and put telemedicine into practice.(4,5)
It is not possible to overcome the burden of interrupted chronic disease follow-ups and missed diagnoses, which have been disrupted during the 3-year period left behind in the normalization era with traditional health care delivery methods.(6,7) Guiding evidence to be produced by the spread of telemedicine practice, the establishment of theoretical, technical, and legal infrastructure of digital health care, and the measurement of the quality and effectiveness of digital clinical services will facilitate the management of the disease burden.(8,9) The evidence-based data that a significant majority of the examinations related to neurological complaints are performed by family physicians has led us to focus on digital solutions in this field and to understand the role of family physicians.(10,11)
1. Neurological Disorders in Primary Care
Neurological disorders (NDs) are heterogeneous diseases that affect the body’s autonomic, peripheral and central nervous system. The non-communicable neurological disorders include migraines, non-migraine headaches, multiple sclerosis, Alzheimer’s disease and other dementias, Parkinson’s disease, epilepsy, and other neurological disorders.(12) Among the NCDs, neurological diseases share a significant proportion and have a devastating effect on patients because neurological disorders are the leading cause of disability and the second leading cause of death worldwide. Common neurological disorders have a social stigma attached with them.
This serves as a major obstacle in identification, management, and counselling of the patients. Added to this is the problem of integrating patients with neurological disorders in the community.(13) Neurological disorders contribute to a significant burden of disease, with 32.9 deaths per 100,000 population and 7.5 million years of life lost (YLLs) (14). The burden of deaths and disability caused by neurological disorders is increasingly being recognized as a global public health challenge, and its burden is set to rise during the next few decades as a result of the population aging.(15)
There is limited available data on the frequency of patients with neurologic conditions visiting their primary care providers (PCPs) and the most common neurologic complaints they present. However, it is well-known that neurologic complaints are prevalent in the general population. According to a survey conducted among family or general practitioners, approximately 9% of patient visits addressed neurologic issues. The most commonly encountered neurologic disorders in these visits included pain (including back pain), headache, peripheral neuropathy, dizziness/vertigo/tinnitus, cerebrovascular disorders, epilepsy, dementia, and Parkinson’s disease.(16) Another study examining both rural and urban primary care settings found that 10.7% of patients presented with neurologic symptoms.(17) Primary care has to play a large role in this aspect.
Primary care plays a crucial role in the management of neurologic disorders. As the first point of contact for patients, primary care providers are often responsible for initial evaluations, diagnosis, and ongoing management of various neurological conditions. They are equipped to address a wide range of neurologic complaints and can provide comprehensive care for patients with conditions such as headache disorders, neuropathies, dizziness/vertigo, movement disorders, epilepsy, and cognitive impairments.(18)
Primary care providers play a significant role in early recognition of neurological symptoms, conducting initial assessments, and determining appropriate referrals to neurologists or other specialists when necessary. They also play a key role in coordinating care, monitoring treatment responses, and providing ongoing support and education to patients and their families. By working closely with neurologists and other healthcare professionals, primary care providers can ensure a multidisciplinary approach to the management of neurologic disorders, promoting optimal patient outcomes and quality of life.(19)
Furthermore, primary care providers could address preventive measures and lifestyle modifications that can help prevent or manage neurologic disorders.(20,21) By promoting healthy behaviors, managing risk factors, and providing patient education, primary care plays a vital role in the prevention and early intervention of neurologic conditions.(22) An analysis of health service delivery data highlights that family physicians are responsible for most of the patient consultations related to neurological complaints.(23) Although neurology specialists tend to handle a larger number of visits for specific conditions such as Parkinson’s disease, epilepsy, and multiple sclerosis, it is essential to recognize the significant role that family physicians play in evaluating and managing complaints associated with vertigo and headaches. Therefore, to optimize clinical services in the field of neurology, it is crucial to involve and collaborate with family physicians.(16)
2. Teleneurology
Neurology telemedicine, also known as “teleneurology,” is a term used to describe the utilization of telemedicine technologies in the field of neurology. Initially, it was predominantly adopted by neurologists. The primary objective of teleneurology is to enhance access to neurologic expertise for patients who face challenges in reaching specialists or have neurologic disabilities that restrict their ability to travel or require time-sensitive care. In addition, telemedicine provides services that may be difficult to deliver through traditional face-to-face consultations, thereby improving the efficiency and effectiveness of existing healthcare services.(24) Wherever there is limited access to neurologic expertise, whether due to a shortage of providers or patients’ impaired mobility, telemedicine presents a promising opportunity to facilitate access to necessary care.
Furthermore, the use of telemedicine for neurological conditions has significantly increased, particularly during the Covid-19 pandemic. Many medical disciplines, including family medicine, have extensively employed telemedicine during this period to address the healthcare needs of patients with neurologic diseases.(25) Teleneurology is frequently employed in emergency stroke and neurocritical care settings, where its application is most common.(26) However, it also plays a significant role in the management of patients with chronic neurologic conditions, including epilepsy.
Telehealth encounters face barriers related to patient acceptance and adoption, technological infrastructure and connectivity, reimbursement and financial considerations, and provider training and support (Table 1). Patients may have concerns about the quality of care, the ability to establish rapport with a remote provider, and the accessibility of necessary technology. Limited access to reliable internet connectivity and digital devices can also hinder the widespread implementation of telehealth.(27)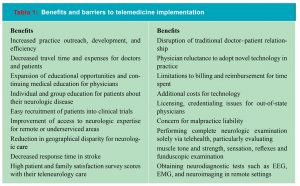
A qualitative study conducted in the United States with the participation of primary care physicians provided a picture of family doctors’ view of the issue. Interview content is structured around the headings of health information technology evaluation, access to care, and health information technology life cycle. After deciphering the data, four main themes were reportedly identified.(28) At first, virtual web-based platform usage experience of both the doctor and the patient was important for the effective implementation of telemedicine applications. There is a need to develop helpful interfaces especially for elderly patients. Secondly, legislation regarding telemedicine should be standardized. Especially in the prescription of controlled substances, studies should be carried out in order to help the patient without harming them.
Moreover, it is unclear which triage rules will apply for telemedicine examinations. The change in standards according to the variable needs during the pandemic makes it difficult for telemedicine to be a permanent part of the daily outpatient consultations. The last important result of the study is that while physicians are concerned that telemedicine service has become a necessity that goes beyond normal working hours, patients see telemedicine as a facilitating factor for control examinations and test result assessments.(28)
Reimbursement policies and coverage limitations pose challenges for healthcare providers, as not all telehealth services may be eligible for reimbursement or may have lower reimbursement rates compared to in-person visits. This can impact the financial viability of telehealth programs and limit their scalability.(28) Provider training and support are essential to ensure that healthcare professionals are proficient in delivering care through telehealth. Providers need training on using telehealth platforms, conducting virtual examinations, and managing potential technical issues. Support in terms of IT infrastructure, troubleshooting, and ongoing education is crucial to enable providers to deliver high-quality care via telehealth.(28)
Interoperability and data sharing among different telehealth platforms and electronic health record systems can be a barrier to seamless integration and coordination of care. Standardization and interoperability efforts are necessary to ensure that patient information can be securely and efficiently transmitted between healthcare providers and systems.(28) Legal and regulatory considerations, including licensure requirements, privacy and security regulations, and compliance with telehealth-specific laws, vary across jurisdictions and can create challenges for providers operating in multiple states or countries.(28)
The existing literature on digital initiatives in the field of neurology highlights the notable aspect of high patient satisfaction. However, it has been found that age and the type of neurological disease significantly influence this satisfaction level. Specifically, individuals over the age of 80 and those diagnosed with movement disorders tend to have relatively lower satisfaction with telemedicine, while patients with epilepsy exhibit higher satisfaction rates.(29) Neurological disorders encompass a broad clinical spectrum, with varying courses and restrictive nature of symptoms. Consequently, patients’ experiences with their specific conditions differ, impacting their attitudes towards clinical interventions such as remote consultations.(29)
From the physicians’ standpoint, the majority overwhelmingly support teleneurological clinical services. However, they tend to prefer phone-based initiatives over more complex video content. Visual assessments that capture the patient’s performance and symptoms play a significant role in diagnosing and monitoring neurological diseases. Therefore, maintaining a remote perspective on information and communication technologies can introduce contradictions and obstacles in clinical practice. There is a clear need for further research to explore the knowledge levels, attitudes, and educational requirements of neurologists and family physicians regarding telemedicine. Such research would provide valuable insights into their perspectives and help address any existing gaps or educational needs in this area.(29)
In addition to the advancements in digital healthcare, the integration of neurologists in primary care can provide valuable support to family physicians.(30,31) This collaboration is essential, especially considering the persistence of “neurophobia” among family physicians, which refers to a reluctance or fear of dealing with neurological conditions.(32,33) By embracing digital transformation, primary care providers can benefit from rapid needs assessments and ongoing medical education, which can help overcome neurophobia and enhance their professional competence.(34) This collaborative approach ensures the uninterrupted delivery of healthcare services and improves patient outcomes.(35,36)
Medical history plays a crucial role in the diagnosis and management of neurological disorders. When evaluating a patient with a neurological condition, obtaining a detailed medical history helps the neurologist understand the patient’s symptoms, their onset, duration, and progression, as well as any associated factors or triggers. 3. Conducting Neurological History and Physical Examination Through Teleconsultation
3.1. Neurological History
A neurological history provides detailed information about a patient’s neurological symptoms, the course of the disease, triggers, risk factors, and the current condition. Here are some important elements that may be included in a neurological history:
Chief Complaints: Specific details about the patient’s symptoms should be inquired. For example, information about the type, location, duration, frequency, and intensity of pain should be gathered. Additionally, any accompanying sensory or motor symptoms such as numbness, weakness, or balance issues should be noted.
Disease History: Information about the onset, progression, and course of the disease should be obtained. Any previous neurological disorders or similar symptoms experienced by the patient should also be documented.
Triggers and Factors: Factors that trigger or exacerbate the symptoms should be investigated. These triggers can include stress, sleep patterns, dietary habits, environmental factors, or medications.
Past Medical Conditions and Surgeries: Previous medical conditions, neurological illnesses, infections, traumas, or surgeries that the patient has experienced should be recorded.
Family History: If there are neurological disorders or genetic conditions present among family members, this information should be documented. Some neurological diseases may have a familial inheritance pattern.
Social and Lifestyle Factors: The patient’s occupation, living environment, habits (such as smoking or alcohol consumption), stress levels, and other lifestyle factors should be considered. These factors can be potential risk factors or triggers for neurological diseases.(37,38)
3.2. Remote Neurological Physical Examination
Studies conducted in the medical literature have consistently shown high patient satisfaction with telemedicine. However, one challenge associated with telemedicine is the question of how to conduct a physical examination when there are physical barriers between the patient and the healthcare provider. To enhance patient satisfaction with telemedicine procedures, involving patients in the physical examination process can be beneficial. Several studies have explored and tested virtual physical examination models, where patients actively participate and follow the physician’s instructions, allowing them to take responsibility and play an active role in the examination process.(39)
Certain aspects of the physical examination, such as verbal instructions for assessing cranial nerve function, can be performed similarly regardless of whether the patient and physician are in the same room or miles apart. However, in areas where quantitative data from vital signs and sensory assessments obtained through auscultation need to be interpreted by the physician, the use of wearable devices becomes crucial in achieving a physical examination of comparable quality to an in-person examination. These devices have the capability to collect data through sensors, process it with their software to generate findings, and transmit them to the physician’s device through telecommunication methods. By utilizing such wearable devices, telemedicine can provide an equivalent level of physical examination as traditional face-to-face encounters.(40)
The integration of telemedicine and e-health applications into everyday medical practices is occurring at a rapid pace. It is crucial to advocate for this inevitable digital transformation process to promote equitable, evidence-based, and high-quality healthcare for everyone. Remote neurological assessment options present opportunities to address the ongoing challenges in neurology healthcare services. In implementing this new approach, it is important to uphold the patient-physician relationship based on patient-centeredness, shared decision-making, and mutual participation, which aligns with the core competencies of the family medicine discipline.(41)
Telemedicine applications, which have been developed for a long time for geographically isolated regions with limited access to resources, have found a rapid application due to the urgent needs arising in the COVID-19 period and a natural validation process has emerged. As a result, although it is not possible to perform a full neurological examination with remote technical support elements, significant experiences have been revealed.
Mental Status
Assessing the mental status of a patient is important in evaluating their cognitive abilities and overall functioning. When conducting remote assessments, the patient’s proficiency in using communication devices can serve as an initial indicator of cognitive competence. Additionally, healthcare providers can ask questions to assess the patient’s orientation to person, place, and time, either directly or with the assistance of a caregiver. Remote administration of cognitive measurement tools, such as the Mini-Mental State Examination (MMSE), is also possible. For example, the patient can write down answers or perform tasks on paper and show them to the camera, providing insights into their cognitive abilities and motor skills.(42,43)
Motor examination
Motor strength assessment during remote physical examinations unavoidably involves some level of subjectivity. To mitigate this issue, conventional measurement scales have been adjusted with descriptive phrases such as “no muscle movement,” “muscle movement without gravity resistance,” “against gravity,” and “beyond gravity.” During the assessment process, patients are given specific instructions. For instance, if it is suspected that a patient’s upper extremity muscle strength surpasses gravity, they may be asked to lift and hold an object of known weight.(42)
Evaluating lower extremity muscle strength can be more intricate. One method involves asking the patient to place a thick book on their knee and then raise their knee toward their chest. If they can accomplish this, it is assumed that their lower extremity motor strength exceeds gravity. Another approach involves instructing the patient to squat and stand up, thereby assessing the resistance of both the quadriceps muscle and knee flexors against gravity. To evaluate the strength of the tibialis anterior and extensor hallucis longus muscles, patients are asked to rise onto their tiptoes and walk a few steps while emphasizing their heels. Likewise, gastrocnemius strength can be assessed by walking on tiptoes.(42)
Sensory examination
The sensory examination poses a challenge in remote physical examinations, particularly when it comes to accurately describing sensations. To overcome this obstacle, visual aids such as dermatome maps can be utilized. These materials help patients identify the specific areas where they are experiencing symptoms. They can be shared with the patient through screen sharing methods. In cases where the patient is unable to identify dermatome areas, body diagrams can be employed as an alternative. This enables the examining physician to differentiate between sensory deficits specific to dermatomes and other types of sensory loss.(42)
Reflex examination
Performing reflex examinations within the context of telemedicine can indeed be challenging. However, certain types of reflexes are more feasible to evaluate remotely. Reflexes such as the biceps, triceps, patellar, and Achilles reflexes can be relatively easily assessed. Having a family member or caregiver present to follow the physician’s instructions is important in these cases. Instead of a reflex hammer, the caregiver can apply pressure with their fingertips as a suitable alternative device for assessing reflexes at home.
When examining for suspected myelopathy, the Babinski reflex can be tested with the patient performing the test themselves in front of the camera. During the examination, the patient is asked to cross their legs so that the foot being tested is resting on the opposite lower extremity. Then, a sharp, key-like tool is drawn from the back of the heel to the front of the toes along the lateral edge of the sole of the foot. In a normal plantar reflex, all five toes bend downward. If the big toe curls upward and the other four toes spread apart, it indicates a positive Babinski reflex. To ensure an effective examination, it is beneficial for the patient to watch educational videos explaining the test beforehand. While reflex examinations may present challenges in telemedicine, with proper adaptations and the involvement of caregivers or family members, certain reflexes can still be evaluated to provide valuable clinical information.
Cranial Nerve Examination
According to various studies, specific methods have been suggested for telemedicine-based cranial nerve examinations: Olfactory Nerve (CN I): Patients can be asked if they have experienced any recent changes or complaints related to their sense of smell. Distinctive odors such as coffee or cologne can be tested by having the patient detect them in front of the screen.(44) Optic Nerve (CN II): Visual acuity can be measured by sharing a visual material containing a Snellen chart with the patient. A full-screen Snellen chart should be displayed on a monitor at a distance of 6 meters. The patient can also perform a visual field test by positioning their arm laterally while zooming in on it to evaluate their peripheral vision.(44)
Oculomotor Nerve (CN III): The patient can stand in front of the screen and follow the physician’s finger movements with their eyes to assess eye movements, looking for diplopia or nystagmus. Pupil reactions can be evaluated by applying a flashlight and conducting the swinging light test.(43) Trochlear Nerve (CN IV): No specific adaptations are required for examining the trochlear nerve through telemedicine. Trigeminal Nerve (CN V): While the motor component of the trigeminal nerve is difficult to assess remotely, the sensory component can be evaluated by showing the patient a face diagram representing the three areas where the nerve receives sensation.(43)
Abducens Nerve (CN VI): No special adaptations are needed for examining the abducens nerve through telemedicine. Facial Nerve (CN VII): Mimic movements can be directed to the patient in front of the camera, and the physician can assess the patient’s facial movements using the House-Brackmann staging system.(43)
Vestibulocochlear Nerve (CN VIII): Assessing the 8th cranial nerve through telemedicine is challenging. Virtual applications of the Rinne and Weber tests are not considered feasible. However, high-quality sound cards and tele-audiogram programs can be used for auditory examinations. Superficial examinations of hearing levels can also be done by evaluating whispering sounds from a family member or caregiver.(44)
Glossopharyngeal Nerve (CN IX): Currently, there are no valid remote examination methods for assessing the glossopharyngeal nerve. The patient’s swallowing function and taste and sensory sensitivity of the posterior third of the tongue can be evaluated through verbal questioning.(44)
Vagus Nerve (CN X): The patient can stand in front of the camera, open their mouth wide, and say “Aah” to assess any uvula deviation.(44) Accessory Nerve (CN XI): As a pure motor nerve, the 11th cranial nerve can be evaluated by instructing the patient to raise their shoulders and turn their head to the right and left.(44) Hypoglossal Nerve (CN XII): The patient can open their mouth and stick out their tongue for assessment. Significant deviation may indicate neuropathy on the ipsilateral side.(44)
4. Technical Support Tools for Remote Tele-neurological Consultations
Wearable devices in neurology create a digital phenotype by collecting and synthesizing diverse bodily measurement data, particularly vital signs.(45, 46,47) This digital phenotype is then transmitted to healthcare providers through online messaging or telecommunications, enabling immediate, synchronized, retrospective, or predictive assessments.(48)
Instant assessment and recording of heart rhythm are crucial for patients with stroke or those at high risk. Smartphones and smartwatches offer adequate equipment for arrhythmia management and proactive approaches.(49) In patients with cognitive disorders, managing comorbid conditions can be challenging, especially in the absence of a caregiver. For instance, a dementia patient with diabetes may have a small applicator placed under their skin to measure and transmit glucose levels, along with transmitter equipment. Processed data can be wirelessly transmitted to smartphones, where user-friendly applications allow patients and physicians to access and interpret the information.(50)
Smartwatch applications sensitive to seizure activity are available for epilepsy patients. These applications can detect epileptic activity during tonic-clonic seizures using sensors that are responsive to involuntary muscle movements. Another device utilizes electrodes placed on the biceps muscle to detect tonic-clonic activity. When necessary, these applications can provide alerts and information to the patient’s relatives, emergency health stations, and physicians via SMS, phone calls, or email. GPS applications are also available to determine the patient’s location for emergency response purposes.(49)
Wearable devices are also useful in assessing movement disorders. For example, in Parkinson’s disease, hardware placed on the back can measure step activity and accelerometer data to evaluate disease progression and movement patterns.(51) Sleep disorders affect a significant portion of the population, and wearable devices can be beneficial in this regard. Wristbands that record physiological parameters detected by sensors are commonly used.(46) Actimeters measure wrist movements, devices evaluate cardiac activity during sleep, and bed-based measurement devices assess thoracic movements and respiratory rate. Additionally, the use of “nearables,” which are wearable sensors attached to everyday items, is increasing. These nearables collect data, such as through Bluetooth, and facilitate wireless data transfer.(52)
Wearable devices hold great promise in supporting remote monitoring and management of neurological disorders. Conditions like stroke, epilepsy, Parkinson’s disease, and sleep disorders can benefit from these devices. However, more research is needed to establish their clinical effectiveness and broader use. Telemedicine programs, especially in primary care, can play a crucial role in generating data for such studies.(46)
In order to achieve equal, accessible, and high-quality neurological healthcare for all, it is crucial to address the challenges and barriers present in telemedicine services. These challenges apply not only to neurology but to all branches of medicine. Some of these barriers include cost-effectiveness issues, limited coverage by traditional insurance models, concerns about cybersecurity and privacy, and the need for sufficient scientific evidence to support new initiatives. Additionally, there are specific challenges in adapting certain aspects of neurological examination, follow-up, and treatment to virtual patient-physician interactions, as well as the need for training primary care physicians in neurology. Overcoming these barriers will be key in realizing the full potential of telemedicine in neurological care.(53)
Conclusion
In conclusion, the utilization of telemedicine in primary care for neurological disorders holds great potential in improving access to high-quality neurological healthcare. It offers convenience, cost-effectiveness, and the ability to reach patients in remote or underserved areas. Telemedicine allows for remote consultations, follow-ups, and monitoring of neurological conditions, providing timely interventions and reducing the burden on patients and healthcare systems. However, challenges such as the need for appropriate technological infrastructure, addressing privacy and security concerns, and ensuring adequate training for healthcare providers must be addressed for successful implementation.
Moreover, further research is needed to demonstrate the efficacy and outcomes of telemedicine in managing neurological disorders. By overcoming these challenges and embracing telemedicine, primary care providers can play a vital role in delivering comprehensive and accessible neurological care to patients, ultimately improving patient outcomes and enhancing the overall healthcare system.
Acknowledgements: We would like to extend our sincere thanks to Dokuz Eylül University Libraries for their support of accessing various databases related to the study.
Confict of interest disclosure: All authors declare that they have no conflicts of interest.
Funding: All authors certify that no funding has been received for the conduct of this study and/or preparation of this manuscript
Authorship contribution: All authors certify that they have participated sufficiently in the work to take public responsibility for the entire content of the manuscript
Referanslar
- Smith A, Thomas E, Snoswell C, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309-13.
- Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions in primary care. Telemed J E Health. 2014;20(9):769-800.
- Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The Impact of the COVID-19 pandemic on outpatient visits: Practices are adapting to the new normal. 2020. https://www.commonwealthfund.org/ publications/2020/ apr/impact-covid-19-outpatient-visits. Accessed on 5/9/2023.
- Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679-81.
- Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract. 2020;8(5):1489-91.
- Heslin MJ, Doherty C, Frimpong JA, Medin DL. Evaluation of the use of telehealth during the COVID-19 pandemic: Observations from the heart of the epicenter. Telemed J E Health. 2021;27(2):195-201.
- Weiner JP, Bandeian S, Hatef E, et al. Development and implementation of a mobile health application to support the COVID-19 pandemic response in an Academic Medical Center. JAMA Netw Open. 2020;3(11):e2022280.
- Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-62.
- Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med. 2020;382(23):e82.
- Rizzuto J, Wingeier R, Bruggimann L, Annoni JM. Development and validation of a mobile phone-based memory assessment in older adults with and without cognitive impairment. JMIR Mhealth Uhealth. 2017;5(2):e25.
- Taylor SW, Taylor RJ. Acceptance and use of telehealth by people with brain injury. Brain Inj. 2005;19(11):777-88.
- Thakur KT, Albanese E, Giannakopoulos P, et al. Neurological Disorders. In “Mental, Neurological, and Substance Use Disorders: Disease Control Priorities”. (eds) Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME. Volume 4. Third Edition. Washington (DC), The International Bank for Reconstruction and Development / The World Bank. 2016.
- GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459-80.
- Pan American Health Organization. The burden of neurological conditions in the Region of the Americas, 2000-2019. Accessed from https://www.paho.org/en/enlace/burden-neurological-conditions on 22/08/2023.
- Feigin VL, Vos T, Nichols E, et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neurol. 2020;19(3):255-65.
- Miller JQ. The neurologic content of family practice. Implications for neurologists. Arch Neurol. 1986;43:286-8.
- Papapetropoulos T, Tsibre E, Pelekoudas V. The neurological content of general practice. J Neurol Neurosurg Psychiatry. 1989;52(4):434-5.
- Xin-Nong L, and Zheng D. The Role of the Primary Care Physician in the Management of Parkinson’s Disease Dementia. In “Dementia in Parkinson’s Disease – Everything You Need to Know” London, IntechOpen. 2021.
- Knowledge and competence of primary care physicians in diagnosis and treatment of nervous system diseases]. Wiad Lek. 2000;53(11-12):629-37.
- Centers for Disease Control and Prevention. 2019. Neurological Disorders Public Health Research, Practice, and Policy. Accessed from https://www.cdc.gov/ncbddd/spanish/healthy-living.html on 22/08/2023.
- World Health Organization. (2004). Neurological disorders: Public health challenges. Accessed from https://www.who.int/mental_health/neurology/chapter_3_burden_neuro_disorders.pdf 22/08/2023.
- Kivipelto M, Ngandu T, Laatikainen T, Winblad B, Soininen H, Tuomilehto J. Risk score for the prediction of dementia risk in 20 years among middle aged people: a longitudinal, population-based study. Lancet Neurol. 2006;5(9):735-41.
- Lin CC, Hill CE, Burke JF, Kerber KA, Hartley SE, Callaghan BC, Skolarus LE. Primary care providers perform more neurologic visits than neurologists among Medicare beneficiaries. J Eval Clin Pract. 2021;27(2):223-7.
- Wechsler LR, Tsao JW, Levine SR, et al. Teleneurology applications: Report of the Telemedicine Work Group of the American Academy of Neurology. Neurology. 2013;80(7):670-6.
- Roy B, Nowak RJ, Roda R, et al. Teleneurology during the COVID-19 pandemic: A step forward in modernizing medical care. J Neurol Sci. 2020;414:116930.
- Ganapathy K. Telemedicine and neurosciences. J Clin Neurosci. 2005;12(8):851-62.
- Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract. 2021;17(2):218-21.
- Rabinowitz G, Cho LD, Benda NC, Goytia C, Andreadis K, Lin JJ, et al. The Telemedicine experience in primary care practices in the United States: Insights from practice leaders. Annals of family medicine. 2023;21(3): 207–12.
- Stavrou M, Lioutas E, Lioutas J, et al. Experiences of remote consulting for patients and neurologists during the COVID-19 pandemic in Scotland. BMJ Neurology Open. 2021;3:e000173.
- Kerchner K, Racette B, & Tychsen L. (2008). Neurology in the medical school curriculum: An integrated approach. Neurology. 2008;71(13): e31-4.
- Jones EL, & Cawley D. Addressing the shortage of neurologists in the United States by training primary care providers to perform neurological screenings. Journal of the American Academy of Physician Assistants. 2013;26(10):52-4.
- Ridsdale L, Massey R, Clark L. Preventing neurophobia in medical students, and so future doctors. Pract Neurol. 2007;7(2):116-23.
- Schon F, Hart P, Fernandez C. Is clinical neurology really so difficult? J Neurol Neurosurg Psychiatry. 2002;72(5):557-9.
- Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: Mixed-methods review. JMIR Med Educ. 2019;5(1):e12515.
- Wootton R. Twenty years of telemedicine in chronic disease management–an evidence synthesis. J Telemed Telecare. 2012;18(4):211-20.
- Davis LE, Coleman J, Harnar J, King MK. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health. 2014;20(5):473-7.
- Beghi E, Gobbi C. Neurological history and physical examination. In “Neurology in Clinical Practice”. Vol 1. 6th ed. Amsterdam, Elsevier. 2020:3-22.
- Victor M, Ropper AH, Samuels MA, Klein JP. Approach to the patient with neurologic disease. In “Adams and Victor’s Principles of Neurology”. 11th ed. New York, McGraw-Hill Education. 2019:1-12.
- Breton M, Sullivan EE, Deville-Stoetzel N, et al. Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Fam Pract. 2021;22(1):192.
- Vijayan V, Connolly JP, Condell J, McKelvey N, Gardiner P. Review of wearable devices and data collection considerations for connected health. Sensors (Basel). 2021;21(16):5589.
- Chirra M, Marsili L, Wattley L, Sokol LL, Keeling E, Maule S, et al. Telemedicine in neurological disorders: Opportunities and challenges. Telemed J E Health. 2019;25(7):541-50.
- Basil G, Luther E, Burks JD, et al. The Focused neurosurgical examination during telehealth visits: Guidelines during the COVID-19 pandemic and beyond. Cureus. 2021;13(2):e13503.
- Dafer RM, Osteraas ND, Biller J. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology Update. Neurology. 2020;94(1):30-8.
- Al Hussona M, Maher M, Chan D, Micieli JA, Jain JD, Khosravani H, et al. The Virtual neurologic exam: Instructional videos and guidance for the COVID-19 era. Can J Neurol Sci. 2020;47(5):598-603.
- Majumder S, Mondal T, Deen MJ. Wearable Sensors for Remote Health Monitoring. Sensors (Basel). 2017;17(1):130.
- Minen MT, Stieglitz EJ. Wearables for neurologic conditions: Considerations for our patients and research limitations. Neurol Clin Pract. 2021;11(4):e537-43.
- Sim I. Mobile devices and health. N Engl J Med. 2019;381:956–68.
- Jain SH, Powers BW, Hawkins JB, Brownstein JS. The digital phenotype. Nat Biotechnol. 2015;33(5):462-3.
- Kakria P, Tripathi NK, Kitipawang P. A Real-time health monitoring system for remote cardiac patients using Smartphone and wearable sensors. Int J Telemed Appl. 2015;2015:373-474.
- Young NP, Burkholder DB, Philpot LM, McKie PM, Ebbert JO. Synchronous neurology-primary care collaboration in a medical home. Neurol Clin Pract. 2020;10(5):388-95.
- Palanisamy P, Padmanabhan A, Ramasamy A, Subramaniam S. Remote patient activity monitoring system by integrating IoT sensors and artificial intelligence techniques. Sensors. 2023;23:5869.
- Contini M, Sarmento A, Gugliandolo P, Leonardi A, Longinotti-Buitoni G, Minella C, et al. Validation of a new wearable device for type 3 sleep test without flowmeter. PLoS ONE. 2021;16(4):e0249470.
- Olszewski C, Thomson S, Pring K, et al. A comparison of telemedicine and in-person neurology visits: what are the factors that patients consider when selecting future visit type? J Neurol. 2022;269(9):5022-37.



